Anti Reflux Surgery
Reflux disease or gastro-oesophageal reflux disease (GORD) is a common problem for many people. It can be quite bothersome and sometimes cause preventable complications. Many people feel just fine after using a small amount of medicine and never need to see a surgeon, but there are some who should come for a discussion to see how we can make things better.
![shutterstock_626849888 [Converted]](https://southernsurgicalcare.com.au/wp-content/uploads/2021/01/shutterstock_626849888-Converted-600x306.png)
The problem with GORD
Reflux disease affects around 40% of adults. Symptoms can range from mild (an occasional ache that can be annoying) through to debilitating (daily bothersome problems despite medicine causing many problems). It is a frequent reason for people seeing a doctor with 2% of GP consults related to GORD and usually these patients need to come back multiple times.
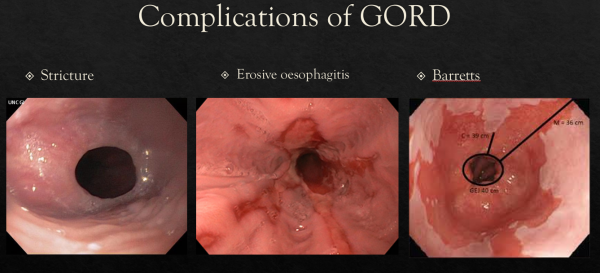
GORD can lead to some serious health problems. Refluxant onto the lower gullet causes irritation and erosions that can bleed (causing anaemia), scar down (preventing swallow) and even perforate (becoming a surgical emergency). Over many years, this irritation can cause changes in the cell type,
becoming something called Barretts Oesophagus… sometimes leading on to oesophageal cancer. Reflux into the throat can also cause problems with the teeth, vocal cords and airways. Many people suffer severe lung infections through reflux and the occasional unlucky few can even scar down the airway.
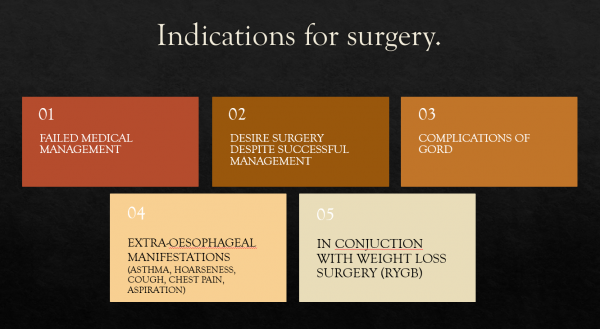
Many of these patients become dependent on an acid lowering medication called Proton Pump Inhibitors. When this is used for many years it can become costly and has recently been shown to have some concerning problems. These include kidney dysfunction, brittle bones, imbalance in the gut microbiome and possibly an increase in a type of stomach cancer.
For these reasons, surgery can be considered for many patients who suffer from reflux disease!
NOTE: HIATUS HERNIA OFTEN MAKES REFLUX WORSE BUT IT IS NOT THE SAME THING.
- See our discussion on the management of hiatus hernia
Indications for Surgery:
Anti-Reflux Surgery
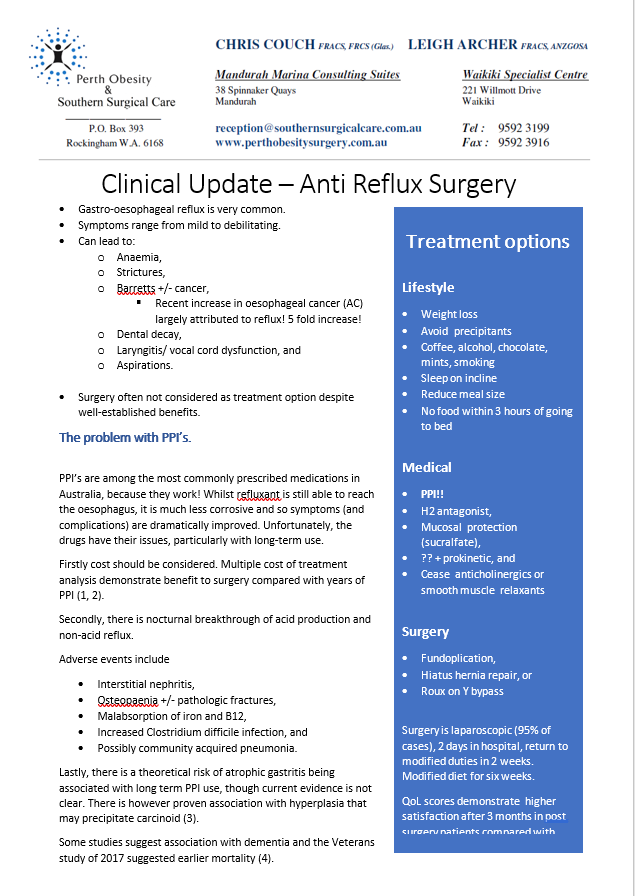
The modern surgical approach to reflux disease is usually with a procedure called a fundoplication. In most cases it is using keyhole and needs 2 to 3 nights in hospital. Modified diet is recommended for around six weeks with step up every 2 weeks from fluids to pureed food and finally a soft diet. Pain is usually not a big problem and most people return to their usual duties after two weeks.
The steps of the procedure:
- General anaesthetic causes the patient to not be aware,
- Keyhole entry with 5 small cuts,
- Separate the upper stomach and lower gullet from the diaphragm and tighten the hole in diaphragm through which the gullet passes,
- Wrap a piece of stomach from one side to the other, creating a pinch valve to minimise reflux, and
- Sometimes a gastroscope is passed down to check repair and see that everything can get through ok.
![shutterstock_1264050388 [Converted]](https://southernsurgicalcare.com.au/wp-content/uploads/2021/01/shutterstock_1264050388-Converted-600x568.png)
Satisfaction
- Functional operation where reflux symptoms are traded for some bloating and slow swallow,
- A small number of people need return to theatre to remove a stitch if it’s difficult to swallow,
- Most people report better quality of life and satisfaction after 3 months.,
- 20% of patients have a recurrence of symptoms and consider a revision operation,
- <1% risk of bleeding, perforation and stunted stomach emptying, and
- Results do vary between operators and best results come from those with a special interest in the problem who do many of the operation.
What to do if things aren’t right afterwards
Everyone is recommended to continue acid lowering medications for a month after the operation. If you don’t feel right after around a month, we will work through what’s happening to figure it out. Often bloating and slow swallow are reported as a recurrence of reflux when in fact it’s the expected effect. In other cases a gastroscope is needed to stretch the area and get everything working again.
The most important thing is to talk to your surgeon about what you are not happy with so we can work it out. Most things can be fixed simply and we want to make sure you have a good outcome now and into the future.

- Gawron AJ, French DD, Pandolfino JE, Howden CW. Economic evaluations of gastroesophageal reflux disease medical management. Pharmacoeconomics. 2014;32(8):745-758. doi:10.1007/s40273-014-0164-8
- Bojke, L., Hornby, E. & Sculpher, M. A Comparison of the Cost Effectiveness of Pharmacotherapy or Surgery (Laparoscopic Fundoplication) in the Treatment of GORD. Pharmacoeconomics25, 829–841 (2007). https://doi.org/10.2165/00019053-200725100-00003Song H, Zhu J, Lu D. Long-term proton pump inhibitor (PPI) use and the development of gastric pre-malignant lesions. Cochrane Database of Systematic Reviews 2014, Issue 12. Art. No.: CD010623. DOI: 10.1002/14651858.CD010623.pub2
- Xie Y, Bowe B, Li T et al. Risk of death among users of Proton Pump Inhibitors: a longitudinal observational cohort study of United States veterans. BMJ Open. 2017;7(6):e015735. Epub 2017 Jul 4.
- Keung C, Hebbard G. The management of gastro-oesophageal reflux disease. Australian Prescriber 2016;39:36-9
- Spechler SJ, Hunter JG, Jones KM et al. Randomized Trial of Medical versus Surgical Treatment for Refractory Heartburn. N Engl J Med. 2019;381(16):1513.
- Lamb PJ, Myers JC, Jamieson GG et al. Long-term outcomes of revisional surgery following laparoscopic fundoplication. Br J Surg. 2009;96(4):391
- Maret-Ouda J, Wahlin K, El-Serag HB, Lagergren J. Association Between Laparoscopic Antireflux Surgery and Recurrence of Gastroesophageal Reflux. 2017;318(10):939.